Big Insurance Uses AI to Quickly Deny Claims, One Man Fights Back with AI App That Quickly Appeals
Health insurance companies in the U.S. have started using AI to analyze and decide claims almost instantly. While this speeds up processing, it often results in rapid denials without human review. Neal Shah, a Raleigh resident, experienced this firsthand when his wife’s chemotherapy drug claim was denied.
At first, Shah thought it was an isolated incident, but after spending hours on phone calls trying to appeal, he realized how common this problem is. He decided to create an AI-powered app that automatically compares claims denial forms with health insurance contracts and drafts appeal letters quickly and accurately.
The Problem with AI-Driven Denials
Before AI, claims denials typically involved a doctor or nurse reviewing the case and providing a reason. Now, many denials happen within seconds through automated AI systems, without human oversight. This makes it harder for patients to challenge wrongful denials.
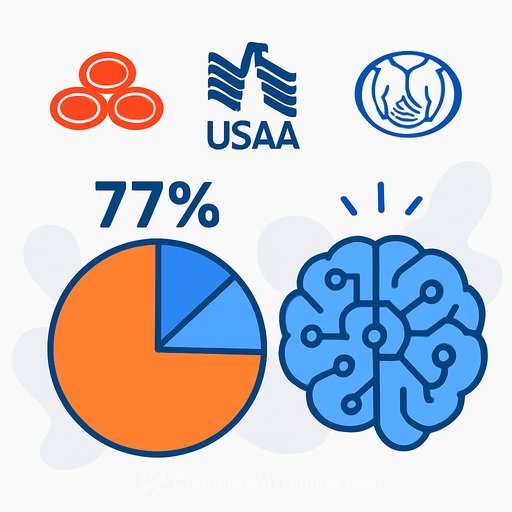
Shah’s research found that 850 million claims get denied annually in the U.S., but fewer than 1% of those denials are appealed. Many people either don’t know they have the right to appeal or don’t know how to start the process.
How Counterforce Health Helps
Shah launched Counterforce Health, a startup offering a free app to help patients appeal denied claims. The app uses AI to scan denial forms, match them against contract terms, and generate persuasive appeal letters.
He partnered with Riyaa Jadhav, who brings experience from both healthcare and business sectors, including work at Johns Hopkins University Hospital. Together, they have developed a tool that boasts a 70% success rate in overturning denials.
Thousands have already used the service, finding it an effective way to push back against quick AI denials. Shah believes that collective pressure from users can help raise awareness and improve the system.
Why Insurance Professionals Should Care
- Understanding how AI is applied in claims adjudication is critical for staying informed about industry trends.
- Tools like Counterforce Health demonstrate how AI can be leveraged not just for denials but also for appeals, changing the balance of power.
- Insurance professionals can benefit from knowing how automated appeals work and how they might influence claim outcomes.
For those interested in learning more about AI applications in insurance and other industries, Complete AI Training offers relevant courses and resources.
Your membership also unlocks: